And yet in Colorado, 8% of deaths have been among the vaccinated since July 1. Less than 1% is good enough odds for me. Why would I live in fear of such an insignificant percentage? I'll leave that for you.0.001% are pretty good odds, wouldn't you say ?
"The CDC reported 6,587 Covid-19 breakthrough cases as of July 26, including 6,239 hospitalizations and 1,263 deaths. At that time, more than 163 million people in the United States were fully vaccinated against Covid-19.
Divide those severe breakthrough cases by the total fully vaccinated population for the result: less than 0.004% of fully vaccinated people had a breakthrough case that led to hospitalization and less than 0.001% of fully vaccinated people died from a breakthrough Covid-19 case"

About 99.999% of fully vaccinated Americans have not had a deadly Covid-19 breakthrough case, CDC data shows | CNN
More than 99.99% of people fully vaccinated against Covid-19 have not had a breakthrough case resulting in hospitalization or death, according to the latest data from the US Centers for Disease Control and Prevention.www.cnn.com
Colleges
- American Athletic
- Atlantic Coast
- Big 12
- Big East
- Big Ten
- Colonial
- Conference USA
- Independents (FBS)
- Junior College
- Mountain West
- Northeast
- Pac-12
- Patriot League
- Pioneer League
- Southeastern
- Sun Belt
- Army
- Charlotte
- East Carolina
- Florida Atlantic
- Memphis
- Navy
- North Texas
- Rice
- South Florida
- Temple
- Tulane
- Tulsa
- UAB
- UTSA
- Boston College
- California
- Clemson
- Duke
- Florida State
- Georgia Tech
- Louisville
- Miami (FL)
- North Carolina
- North Carolina State
- Pittsburgh
- Southern Methodist
- Stanford
- Syracuse
- Virginia
- Virginia Tech
- Wake Forest
- Arizona
- Arizona State
- Baylor
- Brigham Young
- Cincinnati
- Colorado
- Houston
- Iowa State
- Kansas
- Kansas State
- Oklahoma State
- TCU
- Texas Tech
- UCF
- Utah
- West Virginia
- Illinois
- Indiana
- Iowa
- Maryland
- Michigan
- Michigan State
- Minnesota
- Nebraska
- Northwestern
- Ohio State
- Oregon
- Penn State
- Purdue
- Rutgers
- UCLA
- USC
- Washington
- Wisconsin
High Schools
- Illinois HS Sports
- Indiana HS Sports
- Iowa HS Sports
- Kansas HS Sports
- Michigan HS Sports
- Minnesota HS Sports
- Missouri HS Sports
- Nebraska HS Sports
- Oklahoma HS Sports
- Texas HS Hoops
- Texas HS Sports
- Wisconsin HS Sports
- Cincinnati HS Sports
- Delaware
- Maryland HS Sports
- New Jersey HS Hoops
- New Jersey HS Sports
- NYC HS Hoops
- Ohio HS Sports
- Pennsylvania HS Sports
- Virginia HS Sports
- West Virginia HS Sports
ADVERTISEMENT
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
thanks right wing idiots
- Thread starter chevytruck20s
- Start date
And yet in Colorado, 8% of deaths have been among the vaccinated since July 1. Less than 1% is good enough odds for me. Why would I live in fear of such an insignificant percentage? I'll leave that for you.
Do you by chance live in Lauren Boebert's district ?
Never heard of that person.Do you by chance live in Lauren Boebert's district ?
Why do you hate white people? Don’t make racist remarks or you’ll be reported.
I thought thats what we were supposed to be doing... no?
Seems like it based on the posts here and the media telling everyone that white men are the root of all our problems in society.
sorry that happened to your family.I've had my father, 35 years ago, and my grandfather, 70 years ago, die of pancreatic cancer. Yes, if there was an approved vaccine specific to that, I would take it. But that will never happen for any cancer because the "Business" of Cancer (The American Cancer Society, Cancer Treatment Center's of America, Pancreatic Action Network, and just about every Hospital in America with the fanciest of waiting rooms with high dollar fish aquariums in their oncology floors) won't have it. There's just too many jobs and too much money in it for a cure.
Chevy, I fault no one for taking this vaccine. I simply think the odds of survival, unlike a Stage IV cancer diagnosis, are just too great to warrant taking it. I could certainly be wrong. It's just my opinion.
they are now starting trials on mrna vaccines against pancreatic cancer but it sounds complicated.
After a patient has a pancreatic tumor surgically removed, the tumor is genetically sequenced to look for mutations that produce the best neoantigen proteins — that is, the neoantigens that look the most foreign to the immune system. The vaccine is manufactured with mRNA specific to these proteins in that individual’s tumor. While the vaccine is being made, the patient gets a single dose of a checkpoint inhibitor drug. We think checkpoint inhibitors can work in conjunction with these vaccines to boost immune responses to tumors.
When the mRNA vaccine is injected into a person’s bloodstream, it causes immune cells called dendritic cells to make the neoantigen proteins. The dendritic cells also train the rest of the immune system, including T cells, to recognize and attack tumor cells that express these same proteins. With the T cells on high alert to destroy cells bearing these proteins, the cancer may have a lower chance of returning.
In December 2019, we enrolled the first patient in a clinical trial to test if this vaccine was safe. The process to make the vaccines was challenging. For example, the COVID-19 vaccines are not personalized — each vaccine is the same — so it is easy to make them in large batches. The mRNA cancer vaccine must be made individually for each patient based on their tumor. To do this, we must perform a very complex cancer surgery to take out the tumor, ship the sample to Germany, have them sequence it, make the vaccine, and then send back to New York — all within a short timeframe. Thankfully, we were up to the task and just finished enrolling our target total of 20 patients nearly a year ahead of schedule. If all goes well, we plan to conduct larger studies in the future to test mRNA vaccines in cancer patients.
don't want to offend you but you've said your wife almost died from covid and was on a ventilator.And yet in Colorado, 8% of deaths have been among the vaccinated since July 1. Less than 1% is good enough odds for me. Why would I live in fear of such an insignificant percentage? I'll leave that for you.
nobody is saying live in fear. i sure as hell don't. all the shit i've been through in my life, i don't fear much except heights.
lots of stories lately about people asking for the vaccine before they go on a ventilator. doc has to tell them no.
A
anon_fklddvvf21y8b
Guest
No you won't because our great governor says it's up to you. Vote Republican.because of you people refusing to get a little jab in the arm, mask mandates will be back and my kids will have to wear masks at school.
all you cry babies afraid of a little shot in the arm. lmao@ all you fake tough guys.
No offense at all chevy. You are one of the only ones on here that has real experience with how bad the virus can be. Yes, my wife almost died but there was a Dr error that made her case so bad. She feels the same way about shut downs and cloth masks. There are also starting to be more and more stories of those that have been vaccinated catching Covid and ending up in the hospital. Like I said before, we are just beginning to learn about the vaccinated and just how effective it will be. I only hope that you do what you feel is best for you and your family. I will not judge you either way.don't want to offend you but you've said your wife almost died from covid and was on a ventilator.
nobody is saying live in fear. i sure as hell don't. all the shit i've been through in my life, i don't fear much except heights.
lots of stories lately about people asking for the vaccine before they go on a ventilator. doc has to tell them no.
same for you. all the best my fellow cane brother.No offense at all chevy. You are one of the only ones on here that has real experience with how bad the virus can be. Yes, my wife almost died but there was a Dr error that made her case so bad. She feels the same way about shut downs and cloth masks. There are also starting to be more and more stories of those that have been vaccinated catching Covid and ending up in the hospital. Like I said before, we are just beginning to learn about the vaccinated and just how effective it will be. I only hope that you do what you feel is best for you and your family. I will not judge you either way.
i do except when i elect not to vote because i don't agree with or like said candidate.No you won't because our great governor says it's up to you. Vote Republican.
Why do you believe in election fraud? No presidential election in Americam history can be shown to have been rigged. Voting irregularities happen every election but have never even remotely amounted to a degree that would negate a national election. So why do you believe that the only presidential election in American history supposedly rigged just happens to be the one Trump lost?I don’t believe any of those others and had a friends wife on flight 91. The election fraud I absolutely do believe. Also if you want to complain about something complain about why the dumbass in office is still allowing the southern border to be wide open with sock illegals coming in and we have to pay some kind of a price for it. No jab will be going into my arm and no mask will be worn. I’m done and you should be too!
Last edited:
There’s been all kinds of evidence in regards to thing that happened that were said not to have happened. Machines being connected to the internet which were said not to have been. I stayed up and literally watched a massive shift in votes after midnight when supposedly these locations were said to have stopped counting votes. Excuse me for having seen it with my own two eyes. Let me tell you that had this been the reverse with Trump winning and all of the evidence that’s come forward you’d be on your soapbox too. You’ll also never convince me a record breaking 81+ million votes for a guy who could get a thousand people to a rally. I hated Obama but at least he could control a rooms attention. Biden is a total dud. No way Biden pulled more votes than Obama. Just not possible.Why do you believe in election fraud? No presidential election in Americam history can be shown to have been rigged. Voting irregularities happen every election but have never even remotely amounted to a degree that would negate a national election. So why do you believe that the only presidential election in American history supposedly rigged just happens to be the one Trump lost?
If the evidence of fraud was so prevalent, why did every court including SCOTUS dismiss all challenges to overturn election. I watched one program where they claimed a late Biden surge in Pa. was proof of fraud. They failed to mention that the absentee ballets, always heavily Dem, were counted last. Biden rally turnout was intentionally kept low and the record breaking 81+ million votes had more to do with Trump dislike than Biden support! Trump is the best thing to happen for Dems and this will become obvious in the mid-terms! BTW. Cases of the virus spiked in a series of states where Trump held campaign rallies!There’s been all kinds of evidence in regards to thing that happened that were said not to have happened. Machines being connected to the internet which were said not to have been. I stayed up and literally watched a massive shift in votes after midnight when supposedly these locations were said to have stopped counting votes. Excuse me for having seen it with my own two eyes. Let me tell you that had this been the reverse with Trump winning and all of the evidence that’s come forward you’d be on your soapbox too. You’ll also never convince me a record breaking 81+ million votes for a guy who could get a thousand people to a rally. I hated Obama but at least he could control a rooms attention. Biden is a total dud. No way Biden pulled more votes than Obama. Just not possible.
Last edited:
Well, this is great, detailed information chevy. If this leads to, in effect, a cure, then I'm all in. Thanks for sharing this buddy.sorry that happened to your family.
they are now starting trials on mrna vaccines against pancreatic cancer but it sounds complicated.
After a patient has a pancreatic tumor surgically removed, the tumor is genetically sequenced to look for mutations that produce the best neoantigen proteins — that is, the neoantigens that look the most foreign to the immune system. The vaccine is manufactured with mRNA specific to these proteins in that individual’s tumor. While the vaccine is being made, the patient gets a single dose of a checkpoint inhibitor drug. We think checkpoint inhibitors can work in conjunction with these vaccines to boost immune responses to tumors.
When the mRNA vaccine is injected into a person’s bloodstream, it causes immune cells called dendritic cells to make the neoantigen proteins. The dendritic cells also train the rest of the immune system, including T cells, to recognize and attack tumor cells that express these same proteins. With the T cells on high alert to destroy cells bearing these proteins, the cancer may have a lower chance of returning.
In December 2019, we enrolled the first patient in a clinical trial to test if this vaccine was safe. The process to make the vaccines was challenging. For example, the COVID-19 vaccines are not personalized — each vaccine is the same — so it is easy to make them in large batches. The mRNA cancer vaccine must be made individually for each patient based on their tumor. To do this, we must perform a very complex cancer surgery to take out the tumor, ship the sample to Germany, have them sequence it, make the vaccine, and then send back to New York — all within a short timeframe. Thankfully, we were up to the task and just finished enrolling our target total of 20 patients nearly a year ahead of schedule. If all goes well, we plan to conduct larger studies in the future to test mRNA vaccines in cancer patients.
Why do you believe in election fraud? No presidential election in Americam history can be shown to have been rigged. Voting irregularities happen every election but have never even remotely amounted to a degree that would negate a national election. So why do you believe that the only presidential election in American history supposedly rigged just happens to be the one Trump lost?
Here is a very simple mathematical equation explaining a simple reason to raise an eyebrow.
Please, if you can, attempt to explain how simple math is #fakenews for us.
Numbers don't lie.
People and media do.
That is from an old post on Facebook in Dec 2020. There are over 200,000,000 registered voters and 155,485,624 voted in the 2020 election. Numbers don't lie, people do!
Here is a very simple mathematical equation explaining a simple reason to raise an eyebrow.
Please, if you can, attempt to explain how simple math is #fakenews for us.
Numbers don't lie.
People and media do.
African Americans have the highest % of unvaccinated. Hardly a strong Trump-supporting demographic. But don't let the facts get in the way of a good narrative.because of you people refusing to get a little jab in the arm, mask mandates will be back and my kids will have to wear masks at school.
all you cry babies afraid of a little shot in the arm. lmao@ all you fake tough guys.
That is from an old post on Facebook in Dec 2020. There are over 200,000,000 registered voters and 155,485,624 voted in the 2020 election. Numbers don't lie, people do!
Oh ok... that makes total sense and doesn't leave a shred of doubt in my mind at all.
Do you have some sort of reference to confirm 200 million registered voters and 155 million voted?
Use any search engine you wish and type in "133 million registered voters in U.S. " and pick a source.Oh ok... that makes total sense and doesn't leave a shred of doubt in my mind at all.
Do you have some sort of reference to confirm 200 million registered voters and 155 million voted?
The challenges were prematurely presented. The reason why is because there was a window in which certain pieces of info needed to be presented but they couldn’t legally present it without a forensic audit which hadn’t been done yet. Now the forensic audits are returning up substantial evidence and there’s no relief that can be sought since the window is up. Trump can’t boot Biden out of office at this point but that doesn’t mean the election was fair.If the evidence of fraud was so prevalent, why did every court including SCOTUS dismiss all challenges to overturn election. I watched one program where they claimed a late Biden surge in Pa. was proof of fraud. They failed to mention that the absentee ballets, always heavily Dem, were counted last. Biden rally turnout was intentionally kept low and the record breaking 81+ million votes had more to do with Trump dislike than Biden support! Trump is the best thing to happen for Dems and this will become obvious in the mid-terms! BTW. Cases of the virus spiked in a series of states where Trump held campaign rallies!
The challenges were all dismissed because they had no merit. state and federal courts dismissed more than 50 lawsuits presented by Trump and allies saying there was no evidence of widespread fraud. "The Republicans did not provide evidence, just speculation, rumors and hearsay".The challenges were prematurely presented. The reason why is because there was a window in which certain pieces of info needed to be presented but they couldn’t legally present it without a forensic audit which hadn’t been done yet. Now the forensic audits are returning up substantial evidence and there’s no relief that can be sought since the window is up. Trump can’t boot Biden out of office at this point but that doesn’t mean the election was fair.
No, they're left wing idiots. An idiot is an idiot no matter their color. Got it?Down here in Florida, you know right wing idiots, no masks, schools open. BTW only 25% of Blacks vaccinated are they right wing idiots ?
No, they're left wing idiots. An idiot is an idiot no matter their color. Got it?
A guilty conscience needs no accuser.
That's real deep.A guilty conscience needs no accuser.
Lol...lol
Lol..lol
The challenges were all dismissed because they had no merit. state and federal courts dismissed more than 50 lawsuits presented by Trump and allies saying there was no evidence of widespread fraud. "The Republicans did not provide evidence, just speculation, rumors and hearsay".
The election wasn't fair because the other guy won.
Last edited:
You wish they had no merit. They couldn’t get a forensic audit during the time frame and of course states like Georgia purposely kept the forensic audit out of question until the election was settled. Now the forensic audits are taking place there’s massive proven voter fraud.The challenges were all dismissed because they had no merit. state and federal courts dismissed more than 50 lawsuits presented by Trump and allies saying there was no evidence of widespread fraud. "The Republicans did not provide evidence, just speculation, rumors and hearsay".
Sorry, but black and brown people make up 13% of the population unless u are referring to Hispanics as well. All non vaccinated people are idiots.Not right wing or an idiot but this is such an uninformed discussion. Don’t you realize that nearly 2/3 of black and brown Americans have not gotten the vaccine? Black and Brown Americans make up a third of our population. Do the math and get your TDS checked out!
Don’t u mean won!The election wasn't fair because the other guy one.
We can’t move on because healthcare workers are putting their lives on the line as you dumb ass non vaccination people go the ER and infect them. U also are putting children at risk. If u want to take precautions to not get sick, that’s on u, but when it affects my family u are friggin selfish.Excellent post. I neither fault nor criticize ANYONE for choosing to take this or any vaccine. It's totally a matter of choice. But to buy into this characterization that those who choose not to take it, like myself, are selfish uninformed misfits and are delaying things "getting back to normal" is pure ignorance.
Do we ever just accept the fact that this virus and every virus is just going to part of life and you deal with it the best you can WITHOUT the absurd decisions that these lame politicians and supposed scientists have made?
600,000 people will die from cancer this year and every year. That's 50,000 a month. What has science accomplished to reduce that number? Forty years ago it was radiation and chemotherapy. Forty years later it's radiation and chemotherapy. A local news anchor, Jovita Moore on WSB in ATL, was just diagnosed with Glioblastoma, and aggressive brain cancer. It's a death sentence. She's 53 with 3 beautiful kids.
Do we continually want to obsess over this virus with a 98% survival rate? When do we accept the fact that masks, social distancing, and the bullshit lockdowns did absolutely nothing. Why can't we just agree to just fukcing move on from it??
Don't worry pal, I won't go to the ER. My doc got me some Hydroxychloroquine and I take vitamin D daily along with other supplements. I have never masked, social distanced, or changed any element of my life one iota since this insanity began. I suggest you grow a pair and be a good example for your kids by teaching them not to be scared when there's not a damn thing to be scared of. Man up.We can’t move on because healthcare workers are putting their lives on the line as you dumb ass non vaccination people go the ER and infect them. U also are putting children at risk. If u want to take precautions to not get sick, that’s on u, but when it affects my family u are friggin selfish.
Isn't Biden releasing walking Covid Bombs (aka illegal aliens) upon American's for his perceived political gain also "friggin selfish"? Is your family any more or less at risk from an unvaccinated third worlder brought in illegally last month by drug cartels or a 3rd generation US citizen who is not vaccinated due to their honest religious beliefs?
The challenges were prematurely presented. The reason why is because there was a window in which certain pieces of info needed to be presented but they couldn’t legally present it without a forensic audit which hadn’t been done yet. Now the forensic audits are returning up substantial evidence and there’s no relief that can be sought since the window is up. Trump can’t boot Biden out of office at this point but that doesn’t mean the election was fair.
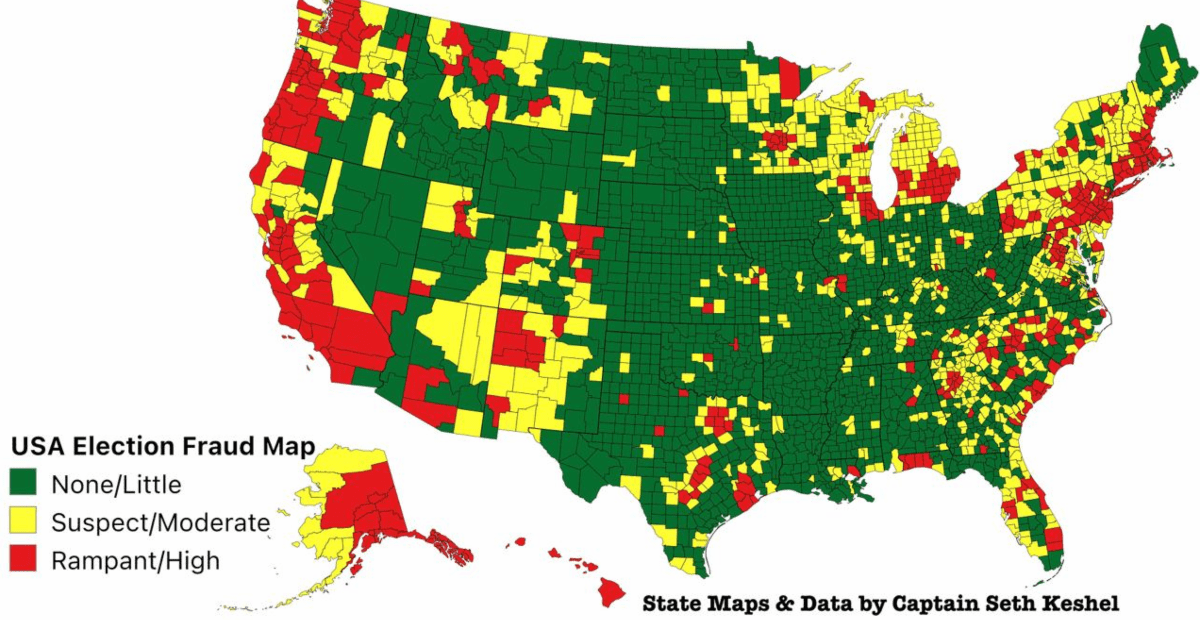
Trump Responds to Bombshell Report on Alleged Voter Fraud Numbers, 'Overwhelming and Election-Changing'
President Trump responded on Tuesday to the report on excess vote numbers from elections expert Seth Keshel, calling them overwhelming and election-changing
 nationalfile.com
nationalfile.com
WrongSorry, but black and brown people make up 13% of the population unless u are referring to Hispanics as well. All non vaccinated people are idiots.
So that's your excuse for not getting a shot? You need to be evaluated for the nearest psych ward.Yeah, then you had the future President and VP saying they wouldn’t get it because Trump had something to do with it. President also said put a mask on for first hundred days mask might be more protection than vaccine. Damm right wing idiots.
Actually, his post makes lots of sense which means you're the one needing some help.God you're a moron...
Show me this CDC report that says 74% of new cases in Mass are from fully vaccinated people. Asking for a friend.Do you have any comment on the CDC report that says that 74% of new cases in Massachusetts were in fully vaccinated people? Will all the people blaming non vaccinated people for the jump in cases be removed from social media for spreading such dangerous misinformation?
Fact: While allegations of voter fraud are frequently bantered around in the news media and by candidates, a large body of research demonstrates very little evidence of voter fraud and clearly not enough to influence the outcome of an election! Don't you find it odd that the only presidential election in history accused of being decided by voter fraud is the one that Trump lost? What a surprise!You wish they had no merit. They couldn’t get a forensic audit during the time frame and of course states like Georgia purposely kept the forensic audit out of question until the election was settled. Now the forensic audits are taking place there’s massive proven voter fraud.
Last edited:
Similar threads
- Replies
- 0
- Views
- 13K
- Replies
- 0
- Views
- 3K
- Replies
- 0
- Views
- 2K
- Replies
- 1
- Views
- 1K
ADVERTISEMENT
ADVERTISEMENT